By Optometrist Scott Brown, Clinical Director at Scotlens
One of the most asked questions I get in my professional services role is what to consider when introducing topography, axial length or both into practice to use for myopia management. Here are some things to consider to help you make these decisions.
Firstly, if you don’t have access to topography or axial length measurements and are not doing anything with myopia management because of this, don’t worry, you do not need either-but that doesn’t mean you should stop reading now! The minimum standard of care is now considered to be that eye care professions should at least mean having a ‘myopia chat’ with patients. This can be advising on lifestyle such as time outdoors and limiting screen use, and also informing patients that optical corrections exist that can reduce myopia progression. A useful non-branded website myopiachat.org is designed to provide this level of information.
The next point I want to make is that having both topography AND axial length is the gold standard.
So, let’s consider the importance and benefits of each…
Benefits of topography
- Enables fitting orthok night lenses. If you currently offer only specs and day lenses as vision correction options, adding night lenses means you offer your existing patients a ‘new’ option. This will attract new patients, because night lenses are patients preferred vision correction option. I often compare practices that don’t offer night lenses to a practice only offering distance and near spectacles or bifocals for presbyopia, and not offering varifocals.
- Enables early detection of keratoconus. Now that corneal cross linking is generally available it is essential that corneal changes are detected and referred early. Topography detects keratoconus years before refraction changes, keratometry changes or retinoscopy. If patients were to have cross linking when detected with topography the current generation of teens could effectively never experience the vision loss that comes with advancing keratoconus. This is my ‘soap box’ as my practice is focused on specialist contact lens fitting so I see all these devastating cases. I would love to see topography considered routine with any eye exam on under 30s.
- It increases understanding of the corneal shape, providing the opportunity for success with more complex contact lens fitting such as custom lenses, sclerals, multifocals and more.
- It makes getting clinical support from contact lens manufacturers or ophthalmologists easier.
So those are quite considerable benefits. But the more important consideration is:
- What are the benefits of GOOD topography?
- Is any topographer fine?
- What functions are needed to make topography worthwhile?
The subtractive function in my opinion is the most important function (Fig. 1)
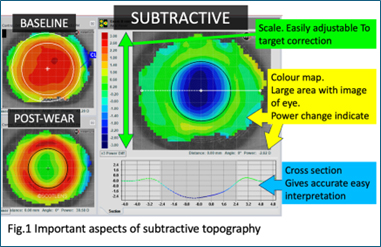
The coloured map display needs to be easy to interpret, the scale of the map needs to be easily adjustable, and the map need to be shown in relation to the image of the eye. This function is the most important because it shows tiny curvature changes in early keratoconus. It also shows the lens fit in nightlens wear, and as fluorescein assessment is in the open eye and is very crude, the accurate lens fit assessment comes from subtractive maps. It shows the treatment zone properties, most importantly the power change on the visual axis (fig. 2)
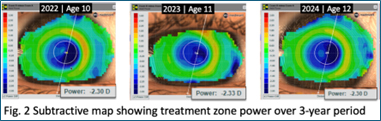
but also diameter and peripheral power. Higher order aberrations can lead to lens fit adjustments that can optimise the myopia control effect.
It can also show power changes with soft lens multi-focals, helping refine lens choice and improve success rates
A key thing to consider is that subtractive maps with night lenses need a baseline map (taken pre-wear). Topography maps are complex 3D model that needs to be compared in the manufacturer’s software. I have patients that have worn night lenses for over 20 years, and at every aftercare I subtract the current map from the 20 year old baseline map (fig. 3)
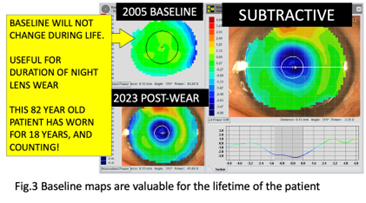
So, if night lenses are going to be part of your practice, choose a topographer with this feature in mind. If you change topographers at a later date, you may need to get all your night lens wearers to wash out, this will mean 4 to 6 weeks of no lens wear…they love their lenses and freedom so much they will not be keen to do this!!
As already mentioned, topography is a 3D capture, hopefully of around a 10mm diameter. The ease of this capture as well as the quality are also important features of good topography. The diameter of the map is key, as when we do a subtractive map, we want to see clear, accurate data across the whole cornea. If capturing the map is difficult, it leads to variability as tear film irregularities start to occur as the patient is staring into the machine and create inaccuracies in the map, making it less reliable.
So, my essentials for a topographer;
- A good subtractive or comparison map (also called compare, B-A) function with the map shown in relation to the eye. If you have a good subtractive function, you will also be able to analyse individual maps well.
- Quick capture with individual captures giving accurate measurement out to around 10mm. Night lenses align the eye from about 7.0mm, so smaller captures reduce the initial lens success and interpretation of lens fit.
- Ability to export and send the full data or an image of the subtractive map to your contact lens supplier or ophthalmology partners.
Other functions such as anterior imaging, meibomian gland assessment, tear film modules, internal contact lens design modules and scleral measurement are less beneficial in night lens and myopia management, so should be considered after establishing the essentials.
Tips on what to ask about if you are considering a buying a topographer.
- Capture- you should be able to quickly capture and analyse maps.
- Baseline map assessment– Placido image, measurement of HVID, map and scale for keratoconus screening (tangential, absolute scale), map and scale for regular corneal assessment (axial, normalised scale)
- Subtractive map assessment- Axial/Refractive subtraction, being able to adjust the scale to interpret the image, tangential subtraction, again being able to adjust the scale to interpret the image.
So, we know topography is essential for orthok night lens fitting but is it essential for myopia management? No. We can still offer lifestyle advice, provide spectacles with myopia control and day lenses with myopia control. We should try and monitor corneal curvatures diligently in under 30s so that we don’t miss early keratoconus, and this may be with Ks or with the crude topography sometime provided by anterior OCT or biometers. If you are planning to start fitting night lenses, then I would recommend selecting a good topographer that you find easy to use.
Benefits of Axial Length Measurement
Axial length is the new kid on the block that is sparking great interest in instrumentation. When we consider the risks associated with myopia it is axial length that is significant rather than the refractive myopia.
Measuring axial length
- Identifies patients with long eyes before myopia develops. This means that we can emphasise lifestyle changes, put patients onto more frequent recall and discuss myopia control options in advance with parents and kids. Early detection is beneficial as axial length grows fastest in the years just before and just as refractive myopia presents. Initiating myopia control early will minimise the eye growth. Axial length is a clear way to communicate why you are advising early myopia control corrections.
- Gives a definitive measurement of eye growth during the myopia development years. This measurement is not subject to any refractive variability like treatment zone power in night lens wear, refractive effect of myopia control soft lenses due to lens position/lens power or patient accommodation.
- This measurement allows tracking of progress. Plotted against average growth curves, clearly demonstrating the benefits of a myopia control device.
- It can also show different growth curve trajectories if combination therapies are going to be offered.
- A significant benefit is for adult myopes. Patients with long eyes can be correctly identified for appropriate monitoring and care. This may include more frequent dilation, Optomap, stricter IOP control etc, than patients with shorter eyes. (Fig.4)
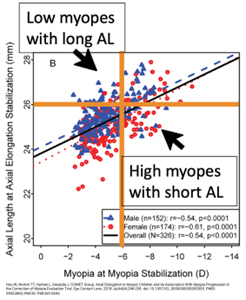
Fig 4. Axial length provides accurate identification of risk
These are considerable benefits. So, are there good or bad axial length measurements?
Bad axial length measurement is no measurement, which is what we do when we are relying on refraction. If the spectacle lens power, day lens power or night lens treatment zone power needs to increase to correct a patient’s vision, we assume the axial length is increasing a corresponding amount. But this is an assumption, so monitoring is less accurate, as is knowing sight loss risks in later life. There is a correlation between spherical equivalent refraction, so -6.00D or greater is associated with sight loss risks as is an axial length of over 26mm. But -2.00D patients can have 27mm long eyes, and -10.00D can have 24mm long eyes.
An option here is to calculate an estimate of the axial length based on keratometry, using an axial length estimator such as this one from Coopervision.
This is only beneficial for myopia control day lens and spectacle patients, and as it is only an estimate, it is not a substitute for accurately measuring axial length, but it can be used as a guide for practitioners who feel this would have value to them.
Good axial length measurement is with interferometry devices. These instruments are traditionally used for IOL assessments, but the technology is now available in more optometric practice friendly options including handheld or combination devices. Ultrasound is generally not used, better than nothing if you happened to have one, like the keratometer versus topographer comparison. Ultrasound is less accurate than cycloplegic autorefraction and needs contact which is not ideal with kids.
Comparing axial length measurement to what I have discussed above with topography there is a key difference. Axial length is a very ‘simple’ measurement of the length of the eye along a single axis. The value will be the same on one device as another, and the value can be put into a tracking spreadsheet or app. This is different to the complex 3D map produced by topographers where comparisons need to be in the same software.
Can topographers or axial length measurements influence the myopia management we offer?
In the UK we can advise on lifestyle, provide specs with myopia control, day lenses with myopia control, night lenses with myopia control or offer repeated low-level red light RLRL. Optometrists don’t have access to atropine.
Lifestyle advice and time out of doors. As an industry, optometry should be all over this. It’s a general health message for fitter, healthier kids. Night lenses and day lenses can help with this after myopia onset, as they provide more freedom for activities than spectacles, but we don’t need either topography or axial length to advise on this component of myopia management.
When advising specs with myopia control, day lenses with mc or night lenses, I tend to advise the most appropriate mode to suit the patient. They all work by the same peripheral defocus optical principle, and they are all comparable in effectiveness. Good patient compliance is more important than advising only one mode for everyone Having a patient enjoy their correction will lead to better compliance and the most effective treatment. Because the efficacy of the 3 modes is proven and roughly equal, I don’t see either topography or axial length altering the myopia management plan.
When topography influences myopia management.
The latest developments and early clinical information suggest that reducing the treatment zone size by reducing the optic zone of the night lens can slow axial length growth compared to a standard night lens design. The established efficacy of myopia control with night lenses is with standard optic sizes. Reducing the treatment zone size can reduce VA. Balancing the treatment zone and VA requires very accurate topography to measure the MDD (equivalent to the ADD in the periphery of the treatment zone), spherical aberration, treatment zone size and treatment zone decentration. Just opting for a small optic zone lens with patients where treatment zone decentration is likely with often lead to poor VA, patient frustration and lost chair time, so good baseline topography assessment is essential.
When Axial Length might influence myopia management.
RLRL is an area I have no experience but am interested to see how it develops. It strikes me as the equivalent to outdoor time that vitamins are for a healthy diet, but it is a new technology that may prove beneficial especially for overly urbanised kids. Measuring axial length enables identifying pre-myopes, meaning that the RLRL treatment may be able to be administered during the period of growth where axial length changes the quickest.
Let’s consider a patient scenario we might encounter in practice.
A young myope was -2.00, 12 months ago.
If they wore specs with myopia control, today they needed -2.75 in the trial frame. No change in topography.
With dual-focus day lenses it was a -0.75 over their -2.00. No change in topography. With night lenses a -0.75 and their treatment zone power on topography was -2.00, unchanged from last year.
They have had an increase in refractive myopia, we are going to give them a -2.75 correction. If they admit not using the correction, we may consider changing to a different mode and topography will confirm no ectasia developing. Each mode is proven to reduce myopia progression, so they should be getting a benefit and not everyone responds equally.
Does the refractive change alter our management? No, we need to correct the full myopia to enable good VA.
Does axial length change our management? If the axial length increase was less than expected for this Rx change at 0mm, or 0.35mm as expected or more than expected at 0.5mm. Whatever the option it doesn’t influence the management.
Summary – Who wins the fight?
If you are holding off from offering myopia management because you don’t have axial length or topography my advice would be don’t. Start getting involved with whatever you have available to you now and start to plan your journey into the other options further down the line. It is a fascinating area of optometry, probably the most exciting topic we will encounter in our careers so don’t miss the opportunity to be a part of it.
I consider topography essential for keratoconic screening and general assessment. If you are not going to offer night lenses, then you can compromise on the topography functionality. If you will be offering night lenses, this can help with funding the cost of the topographer, and I would advise prioritising your topographer to one that is easy to use and produces good comparison maps.
About the author
Optometrist Scott Brown is the Clinical Director of Scotlens | Custom fit contact lenses.